Such as exercise or diet. And metabolism even changes based on external temperature, further making complex attempts to definitively anticipate an experience of thermal comfort by the designer, leaving the inhabitant of the architectural space to engage in a variety of individualistic solutions for regulating the body. Sometimes herniated disk pain can be intermittent. A spin specialist explains why that might be. Share this article via email with one or more people using the form below.
Overview
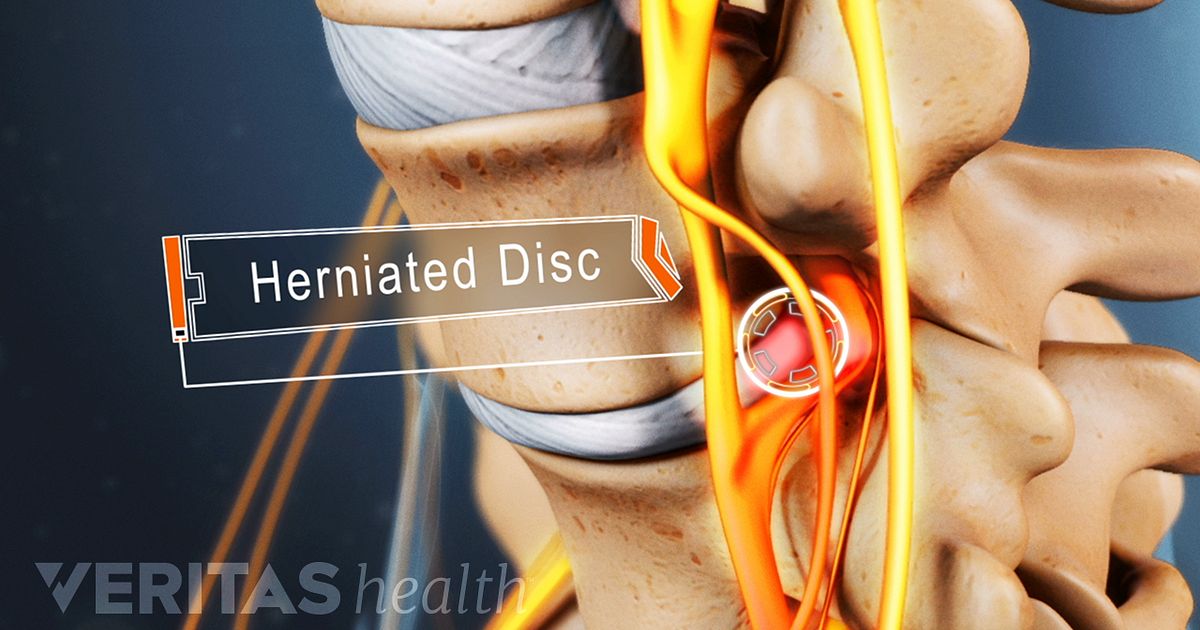
A herniated disc occurs when the gel-like center of a spinal disc ruptures through a weak area in the tough outer wall, similar to the filling being squeezed out of a jelly doughnut. Neck or arm pain, numbness or tingling may result when the disc material touches or compresses a spinal nerve. Treatment with rest, pain medication, spinal injections, and physical therapy is the first step to recovery. Most people improve in 6 weeks and return to normal activity. If symptoms continue, surgery may be recommended.
Anatomy of the discs
Your spine is made of 24 moveable bones called vertebrae. The cervical (neck) section of the spine supports the weight of your head (approximately 10 pounds) and allows you to bend your head forward and backward, from side to side, and rotate 180 degrees. There are 7 cervical vertebrae numbered C1 to C7. The vertebrae are separated by discs, which act as shock absorbers preventing the vertebrae from rubbing together. The outer ring of the disc is called the annulus. It has fibrous bands that attach between the bodies of each vertebra. Each disc has a gel-filled center called the nucleus. At each disc level, a pair of spinal nerves exit from the spinal cord and branch out to your body. Your spinal cord and the spinal nerves act as a 'telephone,' allowing messages, or impulses, to travel back and forth between your brain and body to relay sensation and control movement (see Anatomy of the Spine).
What is a herniated cervical disc?
A herniated disc occurs when the gel-like center of your disc ruptures out through a tear in the tough disc wall (annulus) (Fig. 1). The gel material is irritating to your spinal nerves, causing something like a chemical irritation. The pain is a result of spinal nerve inflammation and swelling caused by the pressure of the herniated disc. Over time, the herniation tends to shrink and you may experience partial or complete pain relief. In most cases, if neck and/or arm pain is going to resolve it will do so in about 6 weeks.
Different terms may be used to describe a herniated disc. A bulging disc (protrusion) occurs when the disc annulus remains intact, but forms an outpouching that can press against the nerves. A true herniated disc (also caimg-fluidd or slipped disc) occurs when the disc annulus cracks or ruptures, allowing the gel-filled center to squeeze out. Sometimes the herniation is so severe that a free fragment occurs, meaning a piece has broken completely free from the disc and is in the spinal canal.

What are the symptoms?
Symptoms of a herniated disc vary greatly depending on the location of the herniation and your own response to pain. If you have a herniated cervical disc, you may feel pain that radiates down your arm and possibly into your hand. You may also feel pain on or near your shoulder blade, and neck pain when turning your head or bending your neck. Sometimes you may have muscle spasms (meaning the muscles tighten uncontrollably). Sometimes the pain is accompanied by numbness and tingling in your arm. You may also have muscle weakness in your biceps, triceps, and handgrip.
You may have first noticed pain when you woke up, without any traumatic event that might have caused injury. Some patients find relief by holding their arm in an elevated position behind their head because this position relieves pressure on the nerve.
What are the causes?
Discs can bulge or herniate because of injury and improper lifting or can occur spontaneously. Aging plays an important role. As you get older, your discs dry out and become harder. The tough fibrous outer wall of the disc may weaken. The gel-like nucleus may bulge or rupture through a tear in the disc wall, causing pain when it touches a nerve. Genetics, smoking, and a number of occupational and recreational activities lead to early disc degeneration.
Who is affected?
Herniated discs are most common in people in their 30s and 40s, although middle aged and older people are slightly more at risk if they're involved in strenuous physical activity. Only about 8% of herniated discs occur in the neck region.

How is a diagnosis made?
When you first experience pain, consult your family doctor. Your doctor will take a complete medical history to understand your symptoms, any prior injuries or conditions, and determine if any lifestyle habits are causing the pain. Next a physical exam is performed to determine the source of the pain and test for any muscle weakness or numbness.
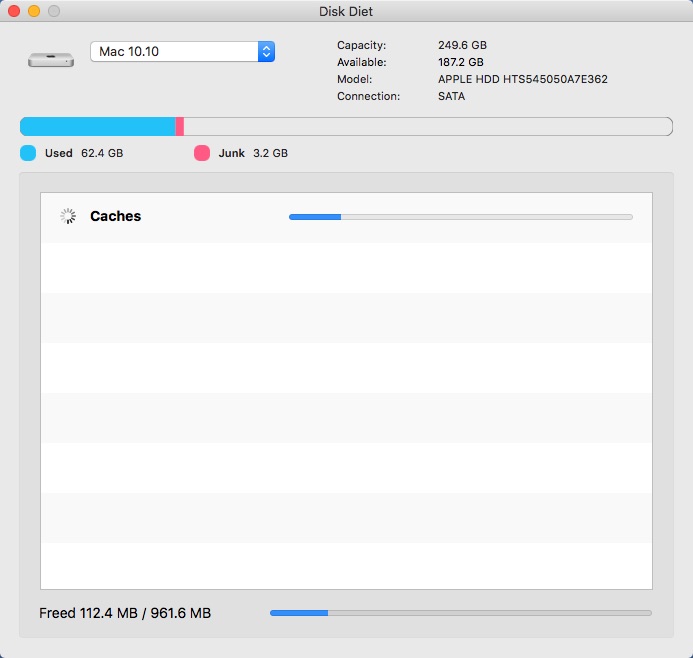
Disk Diet
Your doctor may order one or more of the following imaging studies:
Magnetic Resonance Imaging (MRI) scan is a noninvasive test that uses a magnetic field and radiofrequency waves to give a detailed view of the soft tissues of your spine (Fig. 2). Unlike an X-ray, nerves and discs are clearly visible. It may or may not be performed with a dye (contrast agent) injected into your bloodstream. An MRI can detect which disc is damaged and if there is any nerve compression. It can also detect bony overgrowth, spinal cord tumors, or abscesses.
Myelogram is a specialized X-ray where dye is injected into the spinal canal through a spinal tap. An X-ray fluoroscope then records the images formed by the dye. The dye used in a myelogram shows up white on the X-ray, allowing the physician to view the spinal cord and canal in detail. Myelograms can show a nerve being pinched by a herniated disc, bony overgrowth, spinal cord tumors, and spinal abscesses. A CT scan may follow this test.
Mgh citrix workspace portal. Computed Tomography (CT) scan is a noninvasive test that uses an X-ray beam and a computer to make 2 dimensional images of your spine. It may or may not be performed with a dye (contrast agent) injected into your bloodstream. This test is especially useful for confirming which disc is damaged.
Electromyography (EMG) & Nerve Conduction Studies (NCS): EMG and NCS tests measure the electrical activity of your nerves and muscles. Small needles, or electrodes, are placed in your muscles, and the results are recorded on a special machine. Because a herniated disc causes pressure on the nerve root, the nerve cannot supply feeling and movement to the muscle in a normal manner. These tests can detect nerve damage and muscle weakness.
X-rays view the bony vertebrae in your spine and can tell your doctor if any of them are too close together or whether you have arthritic changes, bone spurs, or fractures. It's not possible to diagnose a herniated disc with this test alone.
What treatments are available?
Conservative nonsurgical treatment is the first step to recovery and may include medication, rest, massage, physical therapy, home exercises, hydrotherapy, chiropractic care, and pain management. Over 95% of people with arm pain due to a herniated disc improve in about six weeks and return to normal activity. If you don't respond to conservative treatment or your symptoms get worse, your doctor may recommend surgery.
Nonsurgical treatments
Self care: In most cases, the pain from a herniated disc will get better within a couple days and completely resolve in 4 to 6 weeks. Restricting your activity, ice/heat therapy, and taking over the counter medications will help your recovery
Medication: Your doctor may prescribe pain relievers, nonsteroidal anti-inflammatory medications (NSAIDs), and steroids. Sometimes muscle relaxers are prescribed for muscle spasms.
Disk Diet
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, naproxen (Alleve, Naprosyn), ibuprofen (Motrin, Nuprin, Advil), and celecoxib (Celebrex), are examples of nonsteroidal anti-inflammatory drugs used to reduce inflammation and relieve pain.
- Analgesics, such as acetaminophen (Tylenol), can relieve pain but don't have the anti-inflammatory effects of NSAIDs. Long-term use of analgesics and NSAIDs may cause stomach ulcers as well as kidney and liver problems.
- Muscle relaxants, such as methocarbamol (Robaxin), carisoprodol (Soma) and cyclobenzaprine (Flexeril), may be prescribed to control muscle spasms.
- Steroids may be prescribed to reduce the swelling and inflammation of the nerves. They are taken orally (as a Medrol dose pack) in a tapering dosage over a five-day period. It has the advantage of providing almost immediate pain relief within a 24-hour period.
Steroid injections: The procedure is done under x-ray fluoroscopy and involves an injection of steroids and a numbing agent into the epidural space of the spine. The medicine is delivered next to the painful area to reduce the swelling and inflammation of the nerves. About 50% of patients will notice relief after an epidural injection, although the results tend to be temporary. Repeat injections may be given to achieve the full effect. Duration of pain relief varies, lasting for weeks or years. Injections are done in conjunction with a physical therapy and/or home exercise program.
Physical therapy: The goal of physical therapy is to help you return to full activity as soon as possible and prevent re-injury. Physical therapists can instruct you on proper posture, lifting, and walking techniques, and they’ll work with you to strengthen and stretch your neck, shoulder, and arm muscles. They’ll also encourage you to stretch and increase the flexibility of your spine and arms. Exercise and strengthening exercises are key elements to your treatment and should become part of your life-long fitness.
Holistic therapies: Some patients find acupuncture, acupressure, yoga, nutrition / diet changes, meditation and biofeedback helpful in managing pain as well as improving overall health.
Surgical treatments
When symptoms progress or do not resolve with conservative treatment, surgery may be an option. Factors such as patient age, how long the problem has persisted, other medical problems, previous neck operations, and expected outcome are considered in planning surgery.
The most common approach to cervical disc surgery is anterior (front of the neck). A posterior (from the back) approach may be performed if you require decompression for other conditions such as stenosis.
- Anterior cervical discectomy & fusion (ACDF): The surgeon makes a small incision in the front of your neck. The neck muscles, vessels and nerves are moved aside to expose the bony vertebra and disc. The portion of the ruptured disc that is pressing on the nerve is removed. After removing the herniated material, the disc space may be filled with a bone graft or cage to create a fusion (Fig. 3). Fusion is the process of joining two or more bones. Over time the graft will fuse to the vertebra above and below to make one solid piece of bone. Metal plates and screws may be used to provide stability during fusion and possibly a better fusion rate.
- Artificial disc replacement: During anterior discectomy a moveable device that mimics a disc’s natural motion is inserted into the damaged joint space. An artificial disc preserves motion, whereas fusion eliminates motion. Made of metal and plastic, they are similar to hip and knee joint implants. Outcomes for artificial disc compared to ACDF (the gold standard) are similar, but cervical disc replacement preserves motion and perhaps avoids adjacent level disease, but this still remains a hypothesis and is not yet proven.
- Minimally invasive microendoscopic discectomy: The surgeon makes a tiny incision in the back of the neck. Small tubes called dilators are used with increasing diameter to enlarge a tunnel to the vertebra. A portion of the bone is removed to expose the nerve root and disc. The surgeon uses either an endoscope or a microscope to remove the ruptured disc. This technique causes less muscle injury than a traditional discectomy.
- Posterior cervical discectomy: The surgeon makes a 1-2 inch incision in the back of your neck. To reach the damaged disc, the spinal muscles are dissected and moved aside to expose the bony vertebra. A section of the bony arch is removed to reach the nerve root and disc space. The portion of the ruptured disc that is compressing the spinal nerve is carefully removed. The spaces through which the nerve roots exit the spine are usually enlarged to prevent future pinching.
Clinical trials
Clinical trials are research studies in which new treatments—drugs, diagnostics, procedures, and other therapies—are tested in people to see if they are safe and effective. Research is always being conducted to improve the standard of medical care. Information about current clinical trials, including eligibility, protocol, and locations, are found on the Web. Studies can be sponsored by the National Institutes of Health (see Clinicaltrials.gov) as well as private industry and pharmaceutical companies (see Centerwatch.com).
Recovery & prevention
Back pain affects 8 of 10 people at some time in their lives, and usually resolves within 6 weeks. A positive mental attitude, regular activity, and a prompt return to work are all very important elements of recovery. If your regular job cannot be done initially, it is in the patient's best interest to return to some kind of modified (light or restricted) duty. Your physician can give prescriptions for such activity for limited periods of time.
The key to avoiding recurrence is prevention:
Degenerative Disk Diet
- Proper lifting techniques (see Self Care for Neck & Back Pain)
- Good posture during sitting, standing, moving, and sleeping
- Appropriate exercise program to strengthen weak abdominal muscles and prevent re-injury
- Healthy weight and lean body mass
- No smoking
Sources & links
If you have more questions, please contact Mayfield Brain & Spine at 800-325-7787 or 513-221-1100.
Spine-health.com
Spineuniverse.com
Glossary
annulus (annulus fibrosis): tough fibrous outer wall of an intervertebral disc.
disc (intervertebral disc): a fiberous cushion that separates spinal vertebrae. Has two parts, a soft gel-like center called the nucleus and a tough fibrous outer wall called the annulus.
discectomy: a type of surgery in which herniated disc material is removed so that it no longer irritates and compresses the nerve root.
nucleus (nucleus pulposus): soft gel-like center of an intervertebral disc.
radiculopathy: refers to any disease affecting the spinal nerve roots. Also used to describe pain along the sciatic nerve that radiates down the leg.
vertebra: (plural vertebrae): one of 33 bones that form the spinal column, they are divided into 7 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 4 coccygeal. Only the top 24 bones are moveable.
updated > 9.2018
reviewed by > Robert Bohinski, MD, PhD, Mayfield Clinic, Cincinnati, Ohio
Mayfield Certified Health Info materials are written and developed by the Mayfield Clinic. This information is not intended to replace the medical advice of your health care provider.
